12.1 Viruses
charles-molnar
Learning Objectives
By the end of this section, you will be able to:
- Describe how viruses were first discovered and how they are detected
- Explain the detailed steps of viral replication
- Describe how vaccines are used in prevention and treatment of viral diseases

No one knows exactly when viruses emerged or from where they came, since viruses do not leave historical footprints such as fossils. Modern viruses are thought to be a mosaic of bits and pieces of nucleic acids picked up from various sources along their respective evolutionary paths. Viruses are acellular, parasitic entities that are not classified within any domain because they are not considered alive. They have no plasma membrane, internal organelles, or metabolic processes, and they do not divide. Instead, they infect a host cell and use the host’s replication processes to produce progeny virus particles. Viruses infect all forms of organisms including bacteria, archaea, fungi, plants, and animals. Living things grow, metabolize, and reproduce. Viruses replicate, but to do so, they are entirely dependent on their host cells. They do not metabolize or grow, but are assembled in their mature form.
Viruses are diverse. They vary in their structure, their replication methods, and in their target hosts or even host cells. While most biological diversity can be understood through evolutionary history, such as how species have adapted to conditions and environments, much about virus origins and evolution remains unknown.
How Viruses Replicate
Viruses were first discovered after the development of a porcelain filter, called the Chamberland-Pasteur filter, which could remove all bacteria visible under the microscope from any liquid sample. In 1886, Adolph Meyer demonstrated that a disease of tobacco plants, tobacco mosaic disease, could be transferred from a diseased plant to a healthy one through liquid plant extracts. In 1892, Dmitri Ivanowski showed that this disease could be transmitted in this way even after the Chamberland-Pasteur filter had removed all viable bacteria from the extract. Still, it was many years before it was proven that these “filterable” infectious agents were not simply very small bacteria but were a new type of tiny, disease-causing particle.
Virions, single virus particles, are very small, about 20–250 nanometers (1 nanometer = 1/1,000,000 mm). These individual virus particles are the infectious form of a virus outside the host cell. Unlike bacteria (which are about 100 times larger), we cannot see viruses with a light microscope, with the exception of some large virions of the poxvirus family (Figure 12.3).
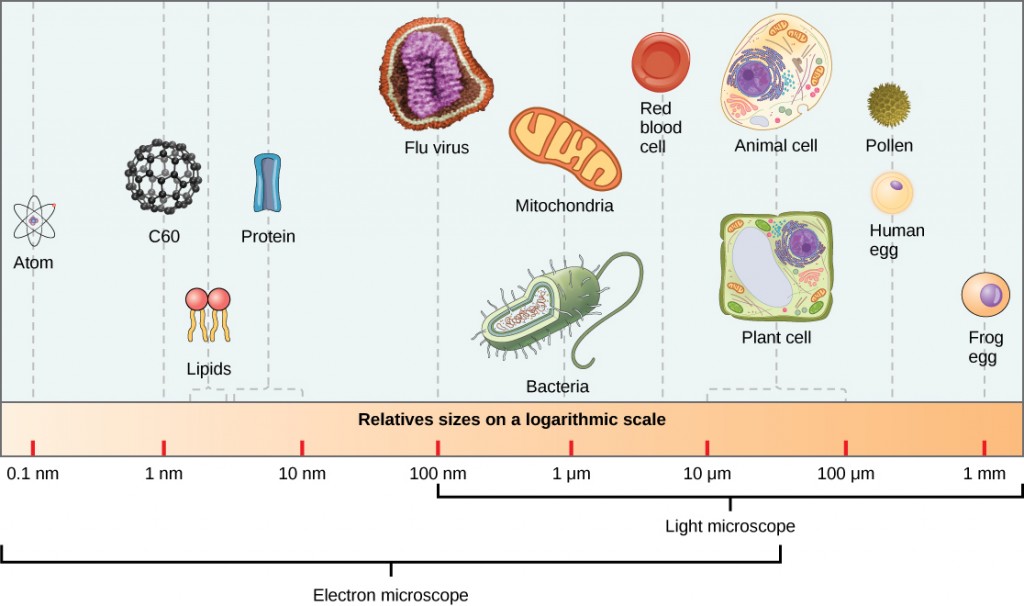
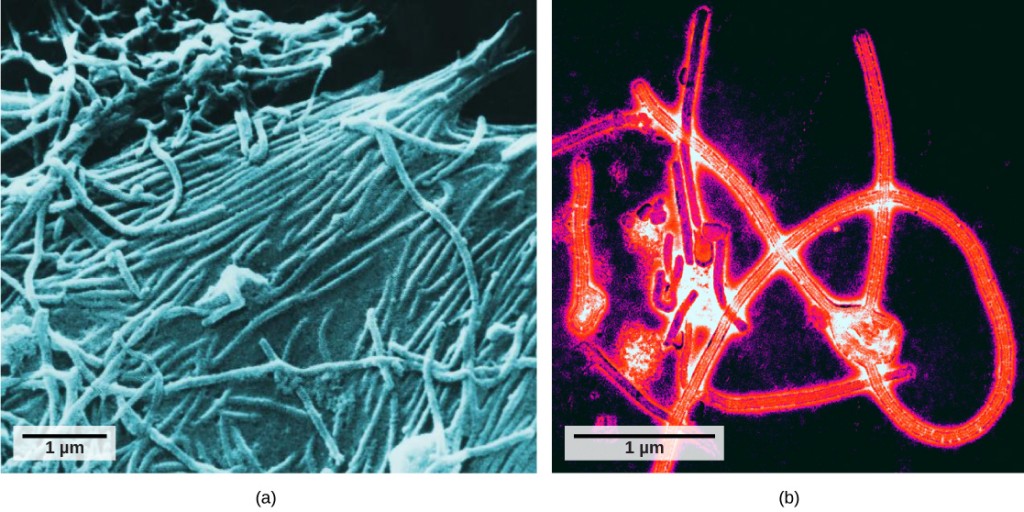
It was not until the development of the electron microscope in the 1940s that scientists got their first good view of the structure of the tobacco mosaic virus (Figure 12.2) and others. The surface structure of virions can be observed by both scanning and transmission electron microscopy, whereas the internal structures of the virus can only be observed in images from a transmission electron microscope (Figure 12.4).
The use of this technology has allowed for the discovery of many viruses of all types of living organisms. They were initially grouped by shared morphology, meaning their size, shape, and distinguishing structures. Later, groups of viruses were classified by the type of nucleic acid they contained, DNA or RNA, and whether their nucleic acid was single- or double-stranded. More recently, molecular analysis of viral replication cycles has further refined their classification.
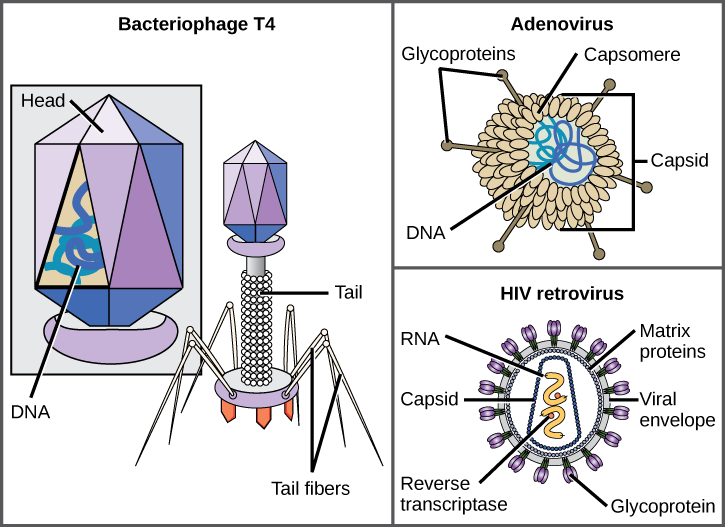
A virion consists of a nucleic-acid core, an outer protein coating, and sometimes an outer envelope made of protein and phospholipid membranes derived from the host cell. The most visible difference between members of viral families is their morphology, which is quite diverse. An interesting feature of viral complexity is that the complexity of the host does not correlate to the complexity of the virion. Some of the most complex virion structures are observed in bacteriophages, viruses that infect the simplest living organisms, bacteria.
Viruses come in many shapes and sizes, but these are consistent and distinct for each viral family (Figure 12.5). All virions have a nucleic-acid genome covered by a protective layer of protein, called a capsid. The capsid is made of protein subunits called capsomeres. Some viral capsids are simple polyhedral “spheres,” whereas others are quite complex in structure. The outer structure surrounding the capsid of some viruses is called the viral envelope. All viruses use some sort of glycoprotein to attach to their host cells at molecules on the cell called viral receptors. The virus exploits these cell-surface molecules, which the cell uses for some other purpose, as a way to recognize and infect specific cell types. For example, the measles virus uses a cell-surface glycoprotein in humans that normally functions in immune reactions and possibly in the sperm-egg interaction at fertilization. Attachment is a requirement for viruses to later penetrate the cell membrane, inject the viral genome, and complete their replication inside the cell.
The T4 bacteriophage, which infects the E. coli bacterium, is among the most complex virion known; T4 has a protein tail structure that the virus uses to attach to the host cell and a head structure that houses its DNA.
Adenovirus, a nonenveloped animal virus that causes respiratory illnesses in humans, uses protein spikes protruding from its capsomeres to attach to the host cell. Nonenveloped viruses also include those that cause polio (poliovirus), plantar warts (papillomavirus), and hepatitis A (hepatitis A virus). Nonenveloped viruses tend to be more robust and more likely to survive under harsh conditions, such as the gut.
Enveloped virions like HIV (human immunodeficiency virus), the causative agent in AIDS (acquired immune deficiency syndrome), consist of nucleic acid (RNA in the case of HIV) and capsid proteins surrounded by a phospholipid bilayer envelope and its associated proteins (Figure 12.5). Chicken pox, influenza, and mumps are examples of diseases caused by viruses with envelopes. Because of the fragility of the envelope, nonenveloped viruses are more resistant to changes in temperature, pH, and some disinfectants than enveloped viruses.
Overall, the shape of the virion and the presence or absence of an envelope tells us little about what diseases the viruses may cause or what species they might infect, but is still a useful means to begin viral classification.
Which of the following statements about virus structure is true?
A) All viruses are encased in a viral membrane.
B) The capsomere is made up of small protein subunits called capsids.
C) DNA is the genetic material in all viruses.
D) Glycoproteins help the virus attach to the host cell.
<!–D–>
Unlike all living organisms that use DNA as their genetic material, viruses may use either DNA or RNA as theirs. The virus core contains the genome or total genetic content of the virus. Viral genomes tend to be small compared to bacteria or eukaryotes, containing only those genes that code for proteins the virus cannot get from the host cell. This genetic material may be single-stranded or double-stranded. It may also be linear or circular. While most viruses contain a single segment of nucleic acid, others have genomes that consist of several segments.
DNA viruses have a DNA core. The viral DNA directs the host cell’s replication proteins to synthesize new copies of the viral genome and to transcribe and translate that genome into viral proteins. DNA viruses cause human diseases such as chickenpox, hepatitis B, and some venereal diseases like herpes and genital warts.
RNA viruses contain only RNA in their cores. To replicate their genomes in the host cell, the genomes of RNA viruses encode enzymes not found in host cells. RNA polymerase enzymes are not as stable as DNA polymerases and often make mistakes during transcription. For this reason, mutations, changes in the nucleotide sequence, in RNA viruses occur more frequently than in DNA viruses. This leads to more rapid evolution and change in RNA viruses. For example, the fact that influenza is an RNA virus is one reason a new flu vaccine is needed every year. Human diseases caused by RNA viruses include hepatitis C, measles, and rabies.
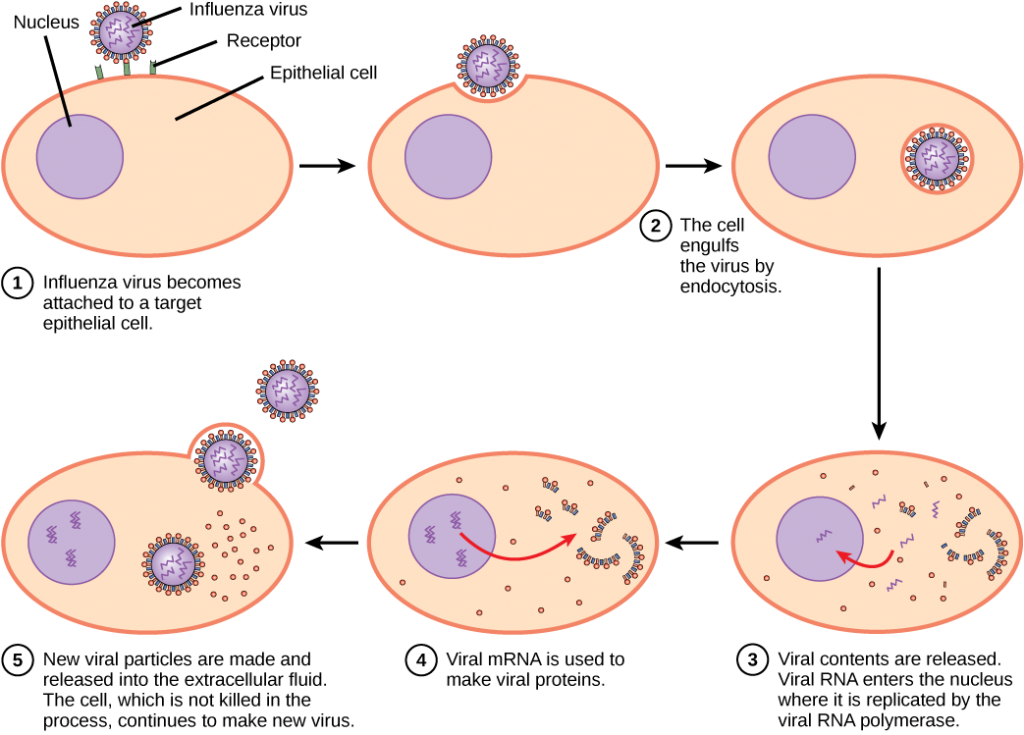
Viruses can be seen as obligate intracellular parasites. The virus must attach to a living cell, be taken inside, manufacture its proteins and copy its genome, and find a way to escape the cell so the virus can infect other cells and ultimately other individuals. Viruses can infect only certain species of hosts and only certain cells within that host. The molecular basis for this specificity is that a particular surface molecule, known as the viral receptor, must be found on the host cell surface for the virus to attach. Also, metabolic differences seen in different cell types based on differential gene expression are a likely factor in which cells a virus may use to replicate. The cell must be making the substances the virus needs, such as enzymes the virus genome itself does not have genes for, or the virus will not be able to replicate using that cell.
Steps of Virus Infections
A virus must “take over” a cell to replicate. The viral replication cycle can produce dramatic biochemical and structural changes in the host cell, which may cause cell damage. These changes, called cytopathic effects, can change cell functions or even destroy the cell. Some infected cells, such as those infected by the common cold virus (rhinovirus), die through lysis (bursting) or apoptosis (programmed cell death or “cell suicide”), releasing all the progeny virions at once. The symptoms of viral diseases result from the immune response to the virus, which attempts to control and eliminate the virus from the body, and from cell damage caused by the virus. Many animal viruses, such as HIV (human immunodeficiency virus), leave the infected cells of the immune system by a process known as budding, where virions leave the cell individually. During the budding process, the cell does not undergo lysis and is not immediately killed. However, the damage to the cells that HIV infects may make it impossible for the cells to function as mediators of immunity, even though the cells remain alive for a period of time. Most productive viral infections follow similar steps in the virus replication cycle: attachment, penetration, uncoating, replication, assembly, and release.
A virus attaches to a specific receptor site on the host-cell membrane through attachment proteins in the capsid or proteins embedded in its envelope. The attachment is specific, and typically a virus will only attach to cells of one or a few species and only certain cell types within those species with the appropriate receptors.
Concept in Action

View this video for a visual explanation of how HIV and influenza attack the body.
Unlike animal viruses, the nucleic acid of bacteriophages is injected into the host cell naked, leaving the capsid outside the cell. Plant and animal viruses can enter their cells through endocytosis, in which the cell membrane surrounds and engulfs the entire virus. Some enveloped viruses enter the cell when the viral envelope fuses directly with the cell membrane. Once inside the cell, the viral capsid is degraded and the viral nucleic acid is released, which then becomes available for replication and transcription.
The replication mechanism depends on the viral genome. DNA viruses usually use host cell proteins and enzymes to make additional DNA that is used to copy the genome or be transcribed to messenger RNA (mRNA), which is then used in protein synthesis. RNA viruses, such as the influenza virus, usually use the RNA core as a template for synthesis of viral genomic RNA and mRNA. The viral mRNA is translated into viral enzymes and capsid proteins to assemble new virions (Figure 12.6). Of course, there are exceptions to this pattern. If a host cell does not provide the enzymes necessary for viral replication, viral genes supply the information to direct synthesis of the missing proteins. Retroviruses, such as HIV, have an RNA genome that must be reverse transcribed to make DNA, which then is inserted into the host’s DNA. To convert RNA into DNA, retroviruses contain genes that encode the virus-specific enzyme reverse transcriptase that transcribes an RNA template to DNA. The fact that HIV produces some of its own enzymes, which are not found in the host, has allowed researchers to develop drugs that inhibit these enzymes. These drugs, including the reverse transcriptase inhibitor AZT, inhibit HIV replication by reducing the activity of the enzyme without affecting the host’s metabolism.
The last stage of viral replication is the release of the new virions into the host organism, where they are able to infect adjacent cells and repeat the replication cycle. Some viruses are released when the host cell dies and other viruses can leave infected cells by budding through the membrane without directly killing the cell.
Influenza virus is packaged in a viral envelope, which fuses with the plasma membrane. This way, the virus can exit the host cell without killing it. What advantage does the virus gain by keeping the host cell alive?
<!–The host cell can continue to make new virus particles.–>
Concept in Action

Click through this tutorial on viruses to identify structures, modes of transmission, replication, and more.
Viruses and Disease
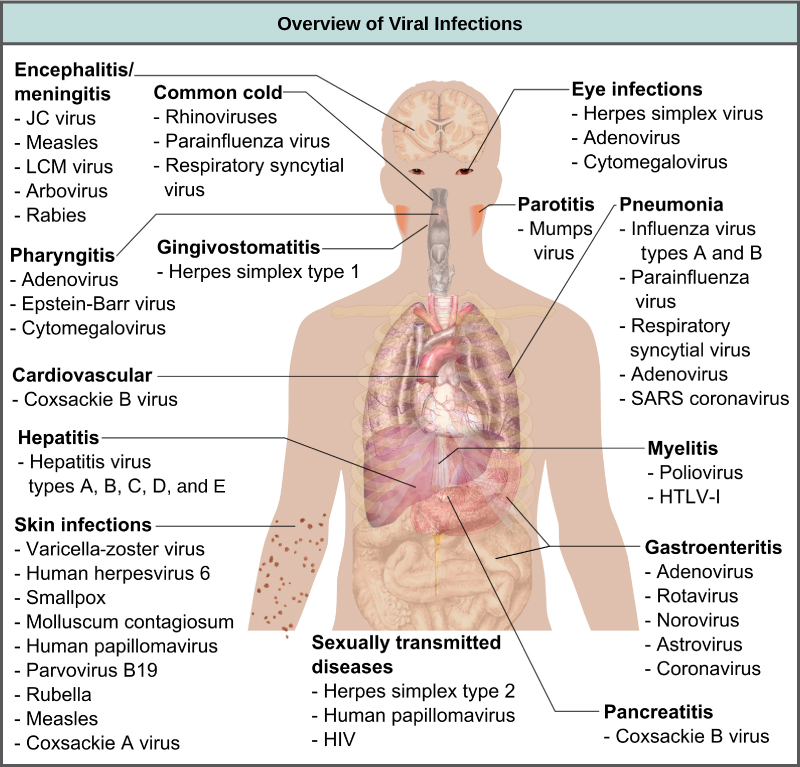
Viruses cause a variety of diseases in animals, including humans, ranging from the common cold to potentially fatal illnesses like meningitis (Figure 12.7). These diseases can be treated by antiviral drugs or by vaccines, but some viruses, such as HIV, are capable of avoiding the immune response and mutating so as to become resistant to antiviral drugs.
Vaccines for Prevention
While we do have limited numbers of effective antiviral drugs, such as those used to treat HIV and influenza, the primary method of controlling viral disease is by vaccination, which is intended to prevent outbreaks by building immunity to a virus or virus family. A vaccine may be prepared using weakened live viruses, killed viruses, or molecular subunits of the virus. In general, live viruses lead to better immunity, but have the possibility of causing disease at some low frequency. Killed viral vaccine and the subunit viruses are both incapable of causing disease, but in general lead to less effective or long-lasting immunity.
Weakened live viral vaccines are designed in the laboratory to cause few symptoms in recipients while giving them immunity against future infections. Polio was one disease that represented a milestone in the use of vaccines. Mass immunization campaigns in the U.S. in the 1950s (killed vaccine) and 1960s (live vaccine) essentially eradicated the disease, which caused muscle paralysis in children and generated fear in the general population when regional epidemics occurred. The success of the polio vaccine paved the way for the routine dispensation of childhood vaccines against measles, mumps, rubella, chickenpox, and other diseases.
Live vaccines are usually made by attenuation (weakening) of the “wild-type” (disease-causing) virus by growing it in the laboratory in tissues or at temperatures different from what the virus is accustomed to in the host. For example, the virus may be grown in cells in a test tube, in bird embryos, or in live animals. The adaptation to these new cells or temperature induces mutations in the virus’ genomes, allowing them to grow better in the laboratory while inhibiting their ability to cause disease when reintroduced into the conditions found in the host. These attenuated viruses thus still cause an infection, but they do not grow very well, allowing the immune response to develop in time to prevent major disease. The danger of using live vaccines, which are usually more effective than killed vaccines, is the low but significant risk that these viruses will revert back to their disease-causing form by back mutations. Back mutations occur when the vaccine undergoes mutations in the host such that it readapts to the host and can again cause disease, which can then be spread to other humans in an epidemic. This happened as recently as 2007 in Nigeria where mutations in a polio vaccine led to an epidemic of polio in that country.
Some vaccines are in continuous development because certain viruses, such as influenza and HIV, have a high mutation rate compared to other viruses or host cells. With influenza, mutation in genes for the surface molecules helps the virus evade the protective immunity that may have been obtained in a previous influenza season, making it necessary for individuals to get vaccinated every year. Other viruses, such as those that cause the childhood diseases measles, mumps, and rubella, mutate so little that the same vaccine is used year after year.
Vaccines and Antiviral Drugs for Treatment
In some cases, vaccines can be used to treat an active viral infection. In the case of rabies, a fatal neurological disease transmitted in the saliva of rabies virus-infected animals, the progression of the disease from the time of the animal bite to the time it enters the central nervous system may be two weeks or longer. This is enough time to vaccinate an individual who suspects being bitten by a rabid animal, and the boosted immune response from the vaccination is enough to prevent the virus from entering nervous tissue. Thus, the fatal neurological consequences of the disease are averted and the individual only has to recover from the infected bite. This approach is also being used for the treatment of Ebola, one of the fastest and most deadly viruses affecting humans, though usually infecting limited populations. Ebola is also a leading cause of death in gorillas. Transmitted by bats and great apes, this virus can cause death in 70–90 percent of the infected within two weeks. Using newly developed vaccines that boost the immune response, there is hope that immune systems of affected individuals will be better able to control the virus, potentially reducing mortality rates.
Another way of treating viral infections is the use of antiviral drugs. These drugs often have limited ability to cure viral disease but have been used to control and reduce symptoms for a wide variety of viral diseases. For most viruses, these drugs inhibit the virus by blocking the actions of one or more of its proteins. It is important that the targeted proteins be encoded for by viral genes and that these molecules are not present in a healthy host cell. In this way, viral growth is inhibited without damaging the host. There are large numbers of antiviral drugs available to treat infections, some specific for a particular virus and others that can affect multiple viruses.
Antivirals have been developed to treat genital herpes (herpes simplex II) and influenza. For genital herpes, drugs such as acyclovir can reduce the number and duration of the episodes of active viral disease during which patients develop viral lesions in their skins cells. As the virus remains latent in nervous tissue of the body for life, this drug is not a cure but can make the symptoms of the disease more manageable. For influenza, drugs like Tamiflu can reduce the duration of “flu” symptoms by one or two days, but the drug does not prevent symptoms entirely. Other antiviral drugs, such as Ribavirin, have been used to treat a variety of viral infections.
By far the most successful use of antivirals has been in the treatment of the retrovirus HIV, which causes a disease that, if untreated, is usually fatal within 10–12 years after being infected. Anti-HIV drugs have been able to control viral replication to the point that individuals receiving these drugs survive for a significantly longer time than the untreated.
Anti-HIV drugs inhibit viral replication at many different phases of the HIV replicative cycle. Drugs have been developed that inhibit the fusion of the HIV viral envelope with the plasma membrane of the host cell (fusion inhibitors), the conversion of its RNA genome to double-stranded DNA (reverse transcriptase inhibitors), the integration of the viral DNA into the host genome (integrase inhibitors), and the processing of viral proteins (protease inhibitors).
When any of these drugs are used individually, the virus’ high mutation rate allows the virus to rapidly evolve resistance to the drug. The breakthrough in the treatment of HIV was the development of highly active anti-retroviral therapy (HAART), which involves a mixture of different drugs, sometimes called a drug “cocktail.” By attacking the virus at different stages of its replication cycle, it is difficult for the virus to develop resistance to multiple drugs at the same time. Still, even with the use of combination HAART therapy, there is concern that, over time, the virus will evolve resistance to this therapy. Thus, new anti-HIV drugs are constantly being developed with the hope of continuing the battle against this highly fatal virus.
Section Summary
Viruses are acellular entities that can usually only be seen with an electron microscope. Their genomes contain either DNA or RNA, and they replicate using the replication proteins of a host cell. Viruses are diverse, infecting archaea, bacteria, fungi, plants, and animals. Viruses consist of a nucleic-acid core surrounded by a protein capsid with or without an outer lipid envelope.
Viral replication within a living cell always produces changes in the cell, sometimes resulting in cell death and sometimes slowly killing the infected cells. There are six basic stages in the virus replication cycle: attachment, penetration, uncoating, replication, assembly, and release. A viral infection may be productive, resulting in new virions, or nonproductive, meaning the virus remains inside the cell without producing new virions.
Viruses cause a variety of diseases in humans. Many of these diseases can be prevented by the use of viral vaccines, which stimulate protective immunity against the virus without causing major disease. Viral vaccines may also be used in active viral infections, boosting the ability of the immune system to control or destroy the virus. Antiviral drugs that target enzymes and other protein products of viral genes have been developed and used with mixed success. Combinations of anti-HIV drugs have been used to effectively control the virus, extending the lifespan of infected individuals.

