24.3. Human Reproductive Anatomy and Gametogenesis
charles-molnar
Learning Objectives
By the end of this section, you will be able to:
- Describe human male and female reproductive anatomies
- Discuss the human sexual response
- Describe spermatogenesis and oogenesis and discuss their differences and similarities
As animals became more complex, specific organs and organ systems developed to support specific functions for the organism. The reproductive structures that evolved in land animals allow males and females to mate, fertilize internally, and support the growth and development of offspring.
Human Reproductive Anatomy
The reproductive tissues of male and female humans develop similarly in utero until a low level of the hormone testosterone is released from male gonads. Testosterone causes the undeveloped tissues to differentiate into male sexual organs. When testosterone is absent, the tissues develop into female sexual tissues. Primitive gonads become testes or ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female; that is, they are homologous structures.
Male Reproductive Anatomy
In the male reproductive system, the scrotum houses the testicles or testes (singular: testis), including providing passage for blood vessels, nerves, and muscles related to testicular function. The testes are a pair of male reproductive organs that produce sperm and some reproductive hormones. Each testis is approximately 2.5 by 3.8 cm (1.5 by 1 in) in size and divided into wedge-shaped lobules by connective tissue called septa. Coiled in each wedge are seminiferous tubules that produce sperm.
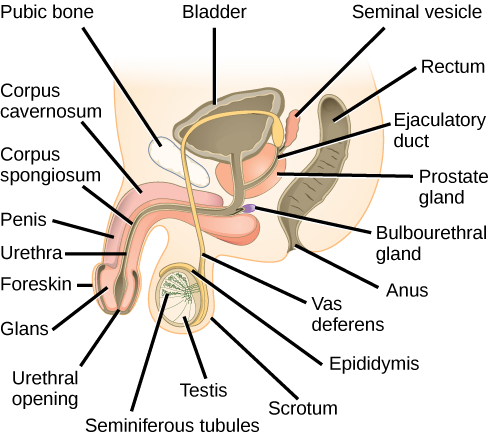
Sperm are immobile at body temperature; therefore, the scrotum and penis are external to the body, as illustrated in Figure 24.8 so that a proper temperature is maintained for motility. In land mammals, the pair of testes must be suspended outside the body at about 2° C lower than body temperature to produce viable sperm. Infertility can occur in land mammals when the testes do not descend through the abdominal cavity during fetal development.
Which of the following statements about the male reproductive system is false?
- The vas deferens carries sperm from the testes to the penis.
- Sperm mature in seminiferous tubules in the testes.
- Both the prostate and the bulbourethral glands produce components of the semen.
- The prostate gland is located in the testes.
Sperm mature in seminiferous tubules that are coiled inside the testes, as illustrated in Figure 24.8. The walls of the seminiferous tubules are made up of the developing sperm cells, with the least developed sperm at the periphery of the tubule and the fully developed sperm in the lumen. The sperm cells are mixed with “nursemaid” cells called Sertoli cells which protect the germ cells and promote their development. Other cells mixed in the wall of the tubules are the interstitial cells of Leydig. These cells produce high levels of testosterone once the male reaches adolescence.
When the sperm have developed flagella and are nearly mature, they leave the testicles and enter the epididymis, shown in Figure 24.8. This structure resembles a comma and lies along the top and posterior portion of the testes; it is the site of sperm maturation. The sperm leave the epididymis and enter the vas deferens (or ductus deferens), which carries the sperm, behind the bladder, and forms the ejaculatory duct with the duct from the seminal vesicles. During a vasectomy, a section of the vas deferens is removed, preventing sperm from being passed out of the body during ejaculation and preventing fertilization.
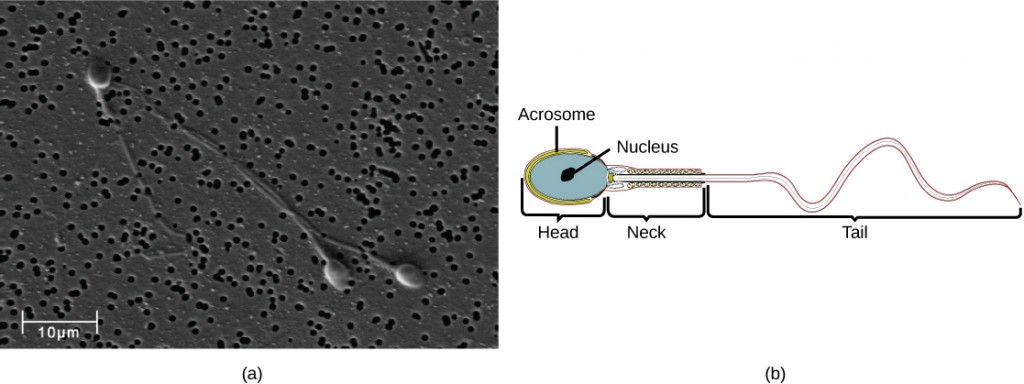
Semen is a mixture of sperm and spermatic duct secretions (about 10 percent of the total) and fluids from accessory glands that contribute most of the semen’s volume. Sperm are haploid cells, consisting of a flagellum as a tail, a neck that contains the cell’s energy-producing mitochondria, and a head that contains the genetic material. Figure 24.9 shows a micrograph of human sperm as well as a diagram of the parts of the sperm. An acrosome is found at the top of the head of the sperm. This structure contains lysosomal enzymes that can digest the protective coverings that surround the egg to help the sperm penetrate and fertilize the egg. An ejaculate will contain from two to five milliliters of fluid with from 50–120 million sperm per milliliter.
The bulk of the semen comes from the accessory glands associated with the male reproductive system. These are the seminal vesicles, the prostate gland, and the bulbourethral gland, all of which are illustrated in Figure 24.8. The seminal vesicles are a pair of glands that lie along the posterior border of the urinary bladder. The glands make a solution that is thick, yellowish, and alkaline. As sperm are only motile in an alkaline environment, a basic pH is important to reverse the acidity of the vaginal environment. The solution also contains mucus, fructose (a sperm mitochondrial nutrient), a coagulating enzyme, ascorbic acid, and local-acting hormones called prostaglandins. The seminal vesicle glands account for 60 percent of the bulk of semen.
The penis, illustrated in Figure 24.8, is an organ that drains urine from the renal bladder and functions as a copulatory organ during intercourse. The penis contains three tubes of erectile tissue running through the length of the organ. These consist of a pair of tubes on the dorsal side, called the corpus cavernosum, and a single tube of tissue on the ventral side, called the corpus spongiosum. This tissue will become engorged with blood, becoming erect and hard, in preparation for intercourse. The organ is inserted into the vagina culminating with an ejaculation. During intercourse, the smooth muscle sphincters at the opening to the renal bladder close and prevent urine from entering the penis. An orgasm is a two-stage process: first, glands and accessory organs connected to the testes contract, then semen (containing sperm) is expelled through the urethra during ejaculation. After intercourse, the blood drains from the erectile tissue and the penis becomes flaccid.
The walnut-shaped prostate gland surrounds the urethra, the connection to the urinary bladder. It has a series of short ducts that directly connect to the urethra. The gland is a mixture of smooth muscle and glandular tissue. The muscle provides much of the force needed for ejaculation to occur. The glandular tissue makes a thin, milky fluid that contains citrate (a nutrient), enzymes, and prostate specific antigen (PSA). PSA is a proteolytic enzyme that helps to liquefy the ejaculate several minutes after release from the male. Prostate gland secretions account for about 30 percent of the bulk of semen.
The bulbourethral gland, or Cowper’s gland, releases its secretion prior to the release of the bulk of the semen. It neutralizes any acid residue in the urethra left over from urine. This usually accounts for a couple of drops of fluid in the total ejaculate and may contain a few sperm. Withdrawal of the penis from the vagina before ejaculation to prevent pregnancy may not work if sperm are present in the bulbourethral gland secretions. The location and functions of the male reproductive organs are summarized in Table 24.1.
| Organ | Location | Function |
|---|---|---|
| Scrotum | External | Carry and support testes |
| Penis | External | Deliver urine, copulating organ |
| Testes | Internal | Produce sperm and male hormones |
| Seminal Vesicles | Internal | Contribute to semen production |
| Prostate Gland | Internal | Contribute to semen production |
| Bulbourethral Glands | Internal | Clean urethra at ejaculation |
Female Reproductive Anatomy
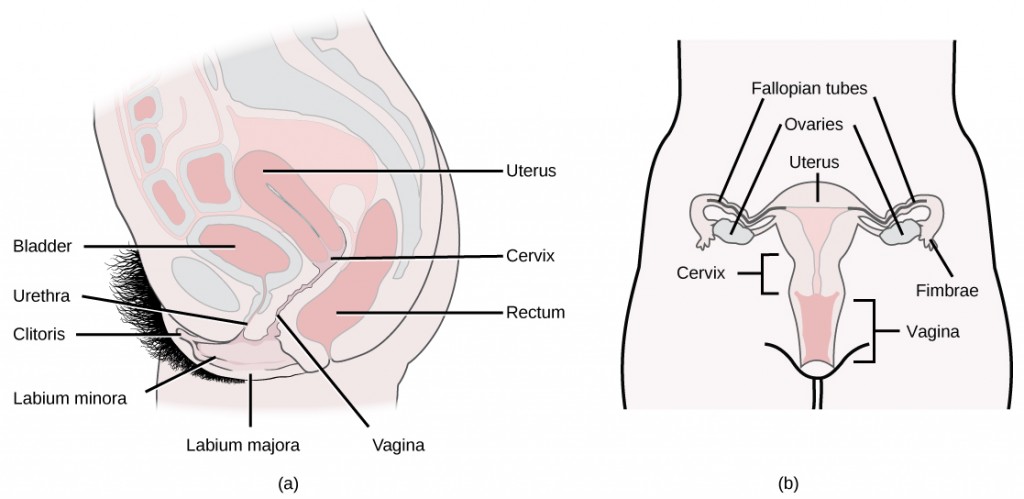
A number of reproductive structures are exterior to the female’s body. These include the breasts and the vulva, which consists of the mons pubis, clitoris, labia majora, labia minora, and the vestibular glands, all illustrated in Figure 24.10. The location and functions of the female reproductive organs are summarized in Table 24.2. The vulva is an area associated with the vestibule which includes the structures found in the inguinal (groin) area of women. The mons pubis is a round, fatty area that overlies the pubic symphysis. The clitoris is a structure with erectile tissue that contains a large number of sensory nerves and serves as a source of stimulation during intercourse. The labia majora are a pair of elongated folds of tissue that run posterior from the mons pubis and enclose the other components of the vulva. The labia majora derive from the same tissue that produces the scrotum in a male. The labia minora are thin folds of tissue centrally located within the labia majora. These labia protect the openings to the vagina and urethra. The mons pubis and the anterior portion of the labia majora become covered with hair during adolescence; the labia minora is hairless. The greater vestibular glands are found at the sides of the vaginal opening and provide lubrication during intercourse.
| Organ | Location | Function |
|---|---|---|
| Clitoris | External | Sensory organ |
| Mons pubis | External | Fatty area overlying pubic bone |
| Labia majora | External | Covers labia minora |
| Labia minora | External | Covers vestibule |
| Greater vestibular glands | External | Secrete mucus; lubricate vagina |
| Breast | External | Produce and deliver milk |
| Ovaries | Internal | Carry and develop eggs |
| Oviducts (Fallopian tubes) | Internal | Transport egg to uterus |
| Uterus | Internal | Support developing embryo |
| Vagina | Internal | Common tube for intercourse, birth canal, passing menstrual flow |
The breasts consist of mammary glands and fat. The size of the breast is determined by the amount of fat deposited behind the gland. Each gland consists of 15 to 25 lobes that have ducts that empty at the nipple and that supply the nursing child with nutrient- and antibody-rich milk to aid development and protect the child.
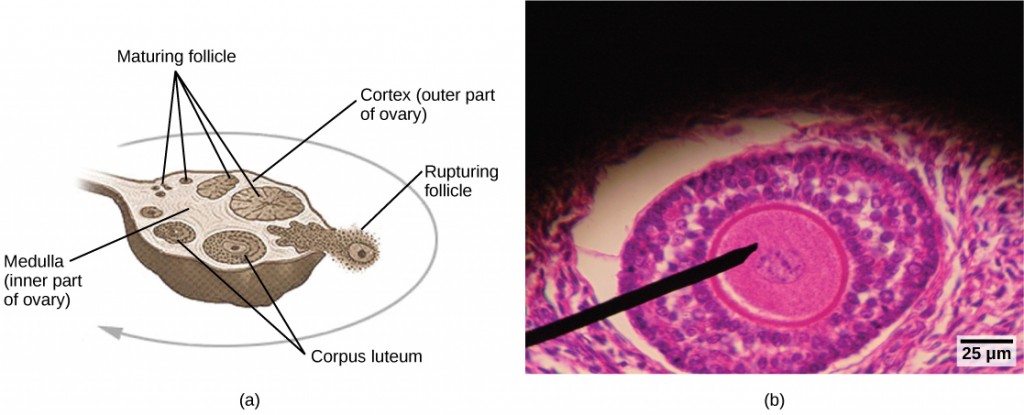
Internal female reproductive structures include ovaries, oviducts, the uterus, and the vagina, shown in Figure 24.10. The pair of ovaries is held in place in the abdominal cavity by a system of ligaments. Ovaries consist of a medulla and cortex: the medulla contains nerves and blood vessels to supply the cortex with nutrients and remove waste. The outer layers of cells of the cortex are the functional parts of the ovaries. The cortex is made up of follicular cells that surround eggs that develop during fetal development in utero. During the menstrual period, a batch of follicular cells develops and prepares the eggs for release. At ovulation, one follicle ruptures and one egg is released, as illustrated in Figure 24.11a.
The oviducts, or fallopian tubes, extend from the uterus in the lower abdominal cavity to the ovaries, but they are not in contact with the ovaries. The lateral ends of the oviducts flare out into a trumpet-like structure and have a fringe of finger-like projections called fimbriae, illustrated in Figure 24.10b. When an egg is released at ovulation, the fimbrae help the non-motile egg enter into the tube and passage to the uterus. The walls of the oviducts are ciliated and are made up mostly of smooth muscle. The cilia beat toward the middle, and the smooth muscle contracts in the same direction, moving the egg toward the uterus. Fertilization usually takes place within the oviducts and the developing embryo is moved toward the uterus for development. It usually takes the egg or embryo a week to travel through the oviduct. Sterilization in women is called a tubal ligation; it is analogous to a vasectomy in males in that the oviducts are severed and sealed.
The uterus is a structure about the size of a woman’s fist. This is lined with an endometrium rich in blood vessels and mucus glands. The uterus supports the developing embryo and fetus during gestation. The thickest portion of the wall of the uterus is made of smooth muscle. Contractions of the smooth muscle in the uterus aid in passing the baby through the vagina during labor. A portion of the lining of the uterus sloughs off during each menstrual period, and then builds up again in preparation for an implantation. Part of the uterus, called the cervix, protrudes into the top of the vagina. The cervix functions as the birth canal.
The vagina is a muscular tube that serves several purposes. It allows menstrual flow to leave the body. It is the receptacle for the penis during intercourse and the vessel for the delivery of offspring. It is lined by stratified squamous epithelial cells to protect the underlying tissue.
Sexual Response during Intercourse
The sexual response in humans is both psychological and physiological. Both sexes experience sexual arousal through psychological and physical stimulation. There are four phases of the sexual response. During phase one, called excitement, vasodilation leads to vasocongestion in erectile tissues in both men and women. The nipples, clitoris, labia, and penis engorge with blood and become enlarged. Vaginal secretions are released to lubricate the vagina to facilitate intercourse. During the second phase, called the plateau, stimulation continues, the outer third of the vaginal wall enlarges with blood, and breathing and heart rate increase.
During phase three, or orgasm, rhythmic, involuntary contractions of muscles occur in both sexes. In the male, the reproductive accessory glands and tubules constrict placing semen in the urethra, then the urethra contracts expelling the semen through the penis. In women, the uterus and vaginal muscles contract in waves that may last slightly less than a second each. During phase four, or resolution, the processes described in the first three phases reverse themselves and return to their normal state. Men experience a refractory period in which they cannot maintain an erection or ejaculate for a period of time ranging from minutes to hours.
Gametogenesis (Spermatogenesis and Oogenesis)
Gametogenesis, the production of sperm and eggs, takes place through the process of meiosis. During meiosis, two cell divisions separate the paired chromosomes in the nucleus and then separate the chromatids that were made during an earlier stage of the cell’s life cycle. Meiosis produces haploid cells with half of each pair of chromosomes normally found in diploid cells. The production of sperm is called spermatogenesis and the production of eggs is called oogenesis.
Spermatogenesis
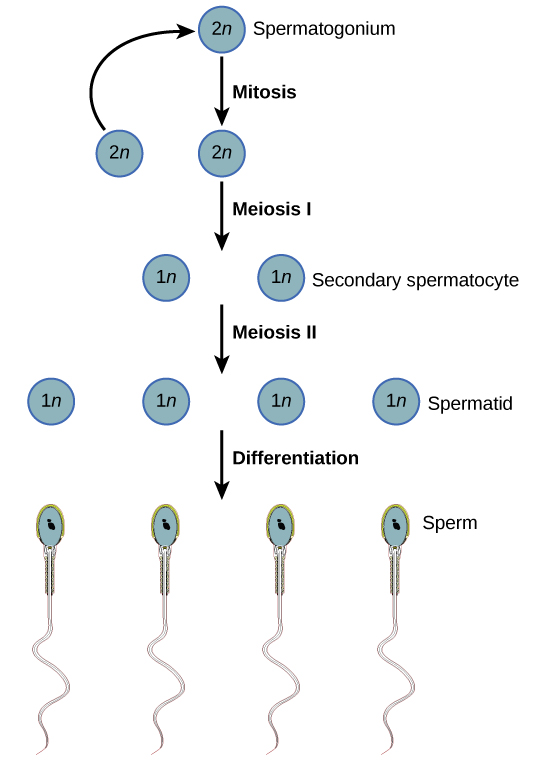
Spermatogenesis, illustrated in Figure 24.12, occurs in the wall of the seminiferous tubules (Figure 24.8), with stem cells at the periphery of the tube and the spermatozoa at the lumen of the tube. Immediately under the capsule of the tubule are diploid, undifferentiated cells. These stem cells, called spermatogonia (singular: spermatagonium), go through mitosis with one offspring going on to differentiate into a sperm cell and the other giving rise to the next generation of sperm.
Meiosis starts with a cell called a primary spermatocyte. At the end of the first meiotic division, a haploid cell is produced called a secondary spermatocyte. This cell is haploid and must go through another meiotic cell division. The cell produced at the end of meiosis is called a spermatid and when it reaches the lumen of the tubule and grows a flagellum, it is called a sperm cell. Four sperm result from each primary spermatocyte that goes through meiosis.
Stem cells are deposited during gestation and are present at birth through the beginning of adolescence, but in an inactive state. During adolescence, gonadotropic hormones from the anterior pituitary cause the activation of these cells and the production of viable sperm. This continues into old age.
Concept in Action

Visit this site to see the process of spermatogenesis.
Oogenesis
Oogenesis, illustrated in Figure 24.13, occurs in the outermost layers of the ovaries. As with sperm production, oogenesis starts with a germ cell, called an oogonium (plural: oogonia), but this cell undergoes mitosis to increase in number, eventually resulting in up to about one to two million cells in the embryo.
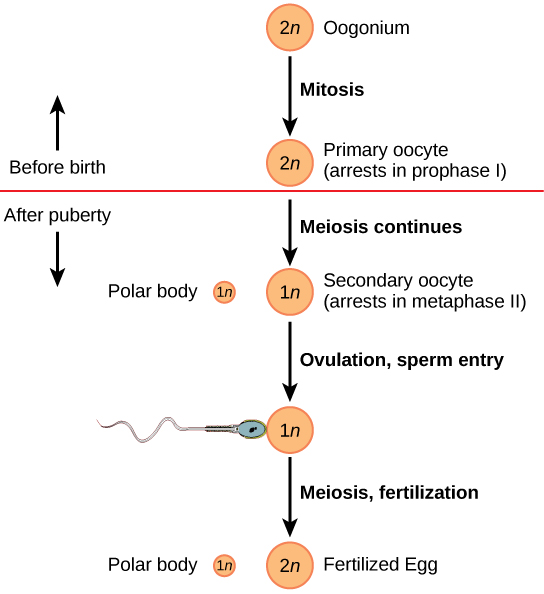
The cell starting meiosis is called a primary oocyte, as shown in Figure 24.13. This cell will start the first meiotic division and be arrested in its progress in the first prophase stage. At the time of birth, all future eggs are in the prophase stage. At adolescence, anterior pituitary hormones cause the development of a number of follicles in an ovary. This results in the primary oocyte finishing the first meiotic division. The cell divides unequally, with most of the cellular material and organelles going to one cell, called a secondary oocyte, and only one set of chromosomes and a small amount of cytoplasm going to the other cell. This second cell is called a polar body and usually dies. A secondary meiotic arrest occurs, this time at the metaphase II stage. At ovulation, this secondary oocyte will be released and travel toward the uterus through the oviduct. If the secondary oocyte is fertilized, the cell continues through the meiosis II, producing a second polar body and a fertilized egg containing all 46 chromosomes of a human being, half of them coming from the sperm.
Egg production begins before birth, is arrested during meiosis until puberty, and then individual cells continue through at each menstrual cycle. One egg is produced from each meiotic process, with the extra chromosomes and chromatids going into polar bodies that degenerate and are reabsorbed by the body.
Summary
As animals became more complex, specific organs and organ systems developed to support specific functions for the organism. The reproductive structures that evolved in land animals allow males and females to mate, fertilize internally, and support the growth and development of offspring. Processes developed to produce reproductive cells that had exactly half the number of chromosomes of each parent so that new combinations would have the appropriate amount of genetic material. Gametogenesis, the production of sperm (spermatogenesis) and eggs (oogenesis), takes place through the process of meiosis.
Exercises
- Which of the following statements about the male reproductive system is false?
- The vas deferens carries sperm from the testes to the penis.
- Sperm mature in seminiferous tubules in the testes.
- Both the prostate and the bulbourethral glands produce components of the semen.
- The prostate gland is located in the testes.
- Sperm are produced in the ________.
- scrotum
- seminal vesicles
- seminiferous tubules
- prostate gland
- Most of the bulk of semen is made by the ________.
- scrotum
- seminal vesicles
- seminiferous tubules
- prostate gland
- Which of the following cells in spermatogenesis is diploid?
- primary spermatocyte
- secondary spermatocyte
- spermatid
- sperm
- Which female organ has the same embryonic origin as the penis?
- clitoris
- labia majora
- greater vestibular glands
- vagina
- Which female organ has an endometrial lining that will support a developing baby?
- labia minora
- breast
- ovaries
- uterus
- How many eggs are produced as a result of one meiotic series of cell divisions?
- one
- two
- three
- four
- Describe the phases of the human sexual response.
- Compare spermatogenesis and oogenesis as to timing of the processes and the number and type of cells finally produced.
Answers
- D
- C
- C
- A
- A
- D
- A
- In phase one (excitement), vasodilation leads to vasocongestion and enlargement of erectile tissues. Vaginal secretions are released to lubricate the vagina during intercourse. In phase two (plateau), stimulation continues, the outer third of the vaginal wall enlarges with blood, and breathing and heart rate increase. In phase three (orgasm), rhythmic, involuntary contractions of muscles occur. In the male, reproductive accessory glands and tubules constrict, depositing semen in the urethra; then, the urethra contracts, expelling the semen through the penis. In women, the uterus and vaginal muscles contract in waves that may last slightly less than a second each. In phase four (resolution), the processes listed in the first three phases reverse themselves and return to their normal state. Men experience a refractory period in which they cannot maintain an erection or ejaculate for a period of time ranging from minutes to hours. Women do not experience a refractory period.
- Stem cells are laid down in the male during gestation and lie dormant until adolescence. Stem cells in the female increase to one to two million and enter the first meiotic division and are arrested in prophase. At adolescence, spermatogenesis begins and continues until death, producing the maximum number of sperm with each meiotic division. Oogenesis continues again at adolescence in batches of oogonia with each menstrual cycle. These oogonia finish the first meiotic division, producing a primary oocyte with most of the cytoplasm and its contents, and a second cell called a polar body containing 23 chromosomes. The second meiotic division results in a secondary oocyte and a second oocyte. At ovulation, a mature haploid egg is released. If this egg is fertilized, it finishes the second meiotic division, including the chromosomes donated by the sperm in the finished cell. This is a diploid, fertilized egg.
Glossary
bulbourethral gland
secretion that cleanses the urethra prior to ejaculation
clitoris
sensory structure in females; stimulated during sexual arousal
labia majora
large folds of tissue covering the inguinal area
labia minora
smaller folds of tissue within the labia majora
oogenesis
process of producing haploid eggs
oviduct(also, fallopian tube)
muscular tube connecting the uterus with the ovary area
penismale reproductive
structure for urine elimination and copulation
prostate gland
structure that is a mixture of smooth muscle and glandular material and that contributes to semen
scrotum
sac containing testes; exterior to the body
semen
fluid mixture of sperm and supporting materials
seminal vesicle
secretory accessory gland in males; contributes to semen
seminiferous tubule
site of sperm production in testes
spermatogenesis
process of producing haploid sperm
testes
pair of reproductive organs in males
uterus
environment for developing embryo and fetus
vagina
muscular tube for the passage of menstrual flow, copulation, and birth of offspring